Think about this for a minute – how many patients do you think the average doctor caters to on a daily basis? And how many total patients does a doctor have under his guidance over the long term? We’re sure you’re going to be shocked by the answer.
The Physicians Foundations, a non-profit organization, surveyed 13,575 doctors in the US in the year 2012. They found that 40% of doctors saw 11 to 20 patients per day, and 27% were visited by a shocking 21 to 30 a day. This number has only increased with more diseases and outbreaks like Covid-19 in the past 2 years.
If that’s not crazy enough, did you know that the average primary-care physician has over 2,300 patients on his panel? That is an astonishing number! But what’s more astonishing is how doctors keep track of all their patients and their needs.
With so many patients to cater to, doctors have established a document system that helps them monitor the progress of each individual. They create documents known as SOAP Notes which have become an essential part of any healthcare system.
In this article, we’ll be covering the meaning of SOAP notes, their importance, and how you can get started creating your own soap notes today! Let’s go!
What are Soap Notes? (Definition)
SOAP notes are defined as the documents used in the medical field to record the interactions between the healthcare provider and the patient. These notes are used by various types of healthcare providers: doctors, psychologists, physicians, therapists, and many more!
SOAP stands for subjective, objective, assessment, and plan. We will elaborate on this in the SOAP note format down below!
But first, let’s take a look at why SOAP notes should be created by every kind of healthcare professional to keep a track of their patients!
Why Should You Create Soap Notes?
Here are a few reasons why soap notes are essential:
1. Progressive Patient Tracking
Soap notes are a way for healthcare professionals like doctors, nurses, and therapists to keep track of a patient’s progress from one visit to the next.
SOAP notes for each client are usually attached or compiled together. Hence, doctors can easily understand the progression of the patient and whether the medicines or treatment plans are making a difference.
2. Consistent Format
SOAP notes have all the important headings already listed that act as cues for the information that has to be recorded. Hence, they make sure that information isn’t left out from a visit to visit.
This consistency will help document all the information that is required on a regular basis and hence…
3. Eases Communication Between Professionals
Medical teams often involve more than one healthcare professional, especially if the patient in question is facing a severe condition or disease. This is because each professional is specialized in a sub-division of medicine.
For example, if a patient has cancer, there are various types of doctors that help: the main oncologist, surgeon, anesthetist, radiologist, nurses, and many more! SOAP notes help convey information between each professional and ensure that nothing is left out or misunderstood.
Now that you’ve understood why it’s so important to create SOAP notes, let’s dive into the SOAP notes creation process!
How to Create Soap Notes? Follow these Steps!
Basic soap notes are easy to create, but hard to master. You want to make sure soap notes are concise, but at the same time detailed enough to make sure important information isn’t left out.
Hence, we have created the perfect format to create your own soap notes. Make sure you cover all the components given below to make your soap notes as comprehensive as possible:
Step 1. Patient Details
Start the document with the name of the patient as well as all their basic details like contact information, email address, etc.
Step 2. Subjective
The S in SOAP stands for subjective information. This is the part of the document that deals with information coming directly from the patient.
This section should start off with the main complaint of the patient, as stated by them. Write down what they are feeling exactly as they describe it.
Components under this include the timeline of onset of symptoms, severity of the symptom, region of the body affected and factors that may have caused the onset.
The patient should also state their medical history that may be relevant to the symptoms they are feeling. Components like family diseases and environmental factors should also be documented here to get a better understanding of the causes of the symptoms.
The last part of this section should be any past or existing medication used by the patient, including dosage and frequency of use. Also include an area for legal or illegal substances that may be abused by the patient. Make sure you explain the importance of being honest and open when filling out this section.
Step 3. Objective
This section should focus on information that the healthcare professional collects from the patient by himself. This includes the on-the-spot diagnosis that is carried out, such as blood pressure, oxygen levels, and all the other essentials.
Whatever tests that are specific to the symptoms that are being shown by the patient should also be documented here. For example, If the patient is showing symptoms of the flu, record the ENT procedures here and the results of the tests performed.
Finally, finish this section off with laboratory tests and imaging like CT or X-ray scans. Essentially, this section should only be facts of the case based on observations and tests.
Step 4. Assessment
This section of the SOAP notes should be the assessment of the subjective and objective observations.
Aim to summarize the case in a few sentences, but make sure you frame them in a way that provides a clear understanding of the problem and what needs to be looked at. Briefly state what the next plans of action would be, but this should be elaborated on thoroughly in the next section.
Step 5. Plan
This section lays out the framework for the next steps that are to be taken by the patient as well as the medical team, if applicable. If there are multiple diagnoses or problems with the patient, list the order in which they need to be treated and how.
Propose how you are going to work towards making the patient healthy. List all the various medicines that need to be taken, along with the doses and frequency. If this is not the first time the patient has paid you a visit, explain if there has been any improvement and what the actions should be,
As stated before, SOAP notes usually involve multiple healthcare professionals, especially in severe cases. hence, these notes are usually sent back and forth between different parties.
This process can be tedious if these notes are made on a traditional document-making software like MS Word, as you can always lose track of the most updated document.
Moreover, it is very hard to send them across if they are made on paper, as multiple changes need to be made, and sending physical files causes logistical problems.
This is why you should use Bit.ai to create the best soap notes.
Bit.ai: The Best Tool For Creating Soap Notes
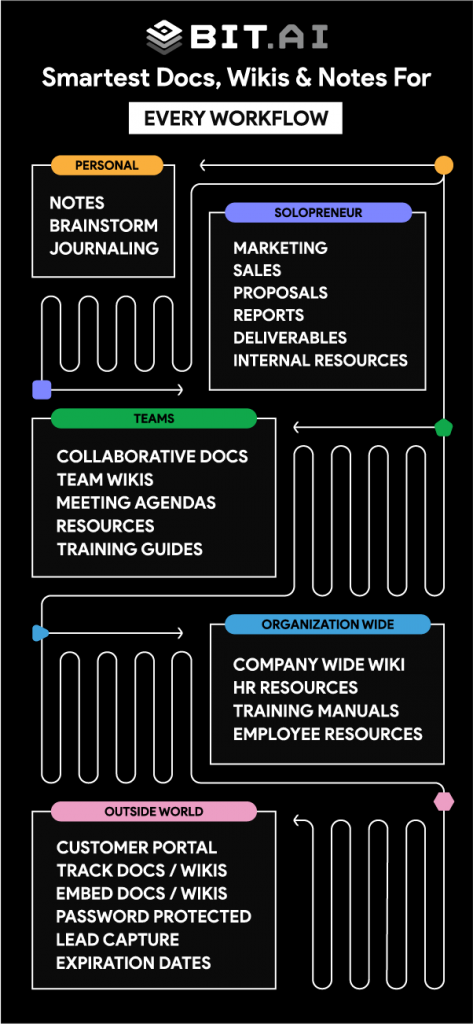
 Bit.ai is the most advanced document collaboration tool that allows you to embed any kind of images, videos, media, and links directly into your documents.
Bit.ai is the most advanced document collaboration tool that allows you to embed any kind of images, videos, media, and links directly into your documents.
This cloud-based platform is perfect for creating various types of documents like soap notes, prescriptions, and more! Here are a few reasons why you should use Bit for SOAP note creation:
1. Collaborate in Real-Time: Bit allows you to work with multiple people in real-time. While creating SOAP notes for severe cases, there may be multiple healthcare professionals involved who may want to put their ideas, observations, and potential treatment solutions down on the document.
With Bit, the different members can work collaboratively through the cloud-based system. This allows all the parties to work faster and add their own content simultaneously, rather than waiting for the other to finish.
2. Negotiate Using Comments: Collaborators can comment on individual pieces of text or phrases. Hence, if a radiologist needs to clarify some pointers written down by the oncologist, he can do it within the document itself. A chat thread can be formed for each comment, so a conversation can occur about a specific problem on the document itself.
This removes the need to go back and forth between the document creating app and a “messenger” app. This also allows the different parties to work remotely, in case their hospital shifts are not aligned. Once the doubt has been sorted out, comments can be “resolved” and the parties can move on to solving the next problem.
3. Create Interactive SOAP Notes: Use Bit to embed images, videos, and any type of media right into your document. This is really useful in SOAP notes because you can embed visual information like organ diagrams, X-ray scans, test results, all in the document.
This eliminates the need to refer to multiple documents on any new windows or links, as everything is present right in one place. You can also embed PDFs within Bit documents, so basically any other information you need is right there in that one document.
Conclusion
As you can see, SOAP notes are essential in documenting the progress of a patient. They are made and compiled to be entered in the patient’s medical records.
SOAP notes prove the contact between the patient and the healthcare provider, allowing for a comprehensive understanding of what the patient is going through and what he needs.
SOAP notes should be used by every type of medical professional. Use Bit to easily collaborate with other professionals and keep a track of SOAP notes.
So what’re you waiting for? Get started with making your SOAP notes today!
Further reads:
11 Best Note-Taking Apps for Better Productivity!
Survey Report: What is it & How to Create it?
9 Powerful Document Editors You Should Use This Year!
Related posts
Bit.ai | Watch to Learn More
What is Bit.ai?
Bit.ai is an innovative AI-driven knowledge and Document Managment suite designed to empower knowledge workers by streamlining the creation of, documents, wikis, and notes. With an intuitive interface and seamless integration, Bit.ai acts as a versatile assistant to help you collaborate, generate, organize, and visualize your ideas effortlessly. Whether you are drafting a report, managing a project, collaborating with your team or clients, or brainstorming new concepts, Bit.ai brings intelligence and creativity to every aspect of your work process.